Grants worth a total of £57,500 have been awarded by the charity Leukaemia and Myeloma Research UK (LMRUK) for two projects that aim to help in the fight against blood cancers.
A record payout for LMRUK’s annual research grant, totalling £35,000, has been made to Dr Neil Rodrigues (pictured above), the principal investigator, and Professor Alex Tonks, co-investigator, at the European Cancer Stem Cell Research Institute at Cardiff University.
The money will help Dr Rodrigues continue his and Professor Tonks’ ground-breaking work into finding a more effective treatment for Acute Myeloid Leukaemia (AML) – a cancer of white blood cells that grow in the bone marrow. In the UK, approximately 2,000 people a year are diagnosed with the condition which, overall, has a poor prognosis.
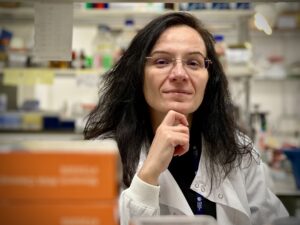 LMRUK has also awarded a research grant of £22,500 to Dr Concetta Bubici, senior lecturer in the College of Health, Medicine and Life Sciences at the Brunel University of London, to continue her work investigating treatment for Myeloma by starving the disease of nutrients, specifically sugar and fat.
LMRUK has also awarded a research grant of £22,500 to Dr Concetta Bubici, senior lecturer in the College of Health, Medicine and Life Sciences at the Brunel University of London, to continue her work investigating treatment for Myeloma by starving the disease of nutrients, specifically sugar and fat.
Dr Bubici said she was very grateful for the LMRUK grant which would allow her to further her studies on Myeloma and help identify the disease’s underlying causes, leading to more effective target drugs.
The Lister Wilder Research Grant awarded to Dr Bubici comes from money raised by Lister Wilder, a horticultural, agricultural and forestry machinery dealership with branches across the south of England. The money was raised by the company after one of their colleagues was diagnosed with blood cancer.
Dr Rodrigues said he was “honoured” to be the recipient of the award made directly by LMRUK for his work on AML in support of the research project titled: “Understanding ZEB1 mediated regulation of human Acute Myeloid Leukaemia (AML) to leverage novel therapeutics in poor prognosis AML.”
He said the project, which was initiated in 2016, showed a gene called ZEB1 was a ‘master switch’ capable of activating ‘flags’ on leukaemia cells. Those ‘flags’ are potential new therapeutic targets in AML.
Dr Rodrigues said: “We’ve identified one ‘flag’ that we are aiming at taking down, but we want to identify a wide range of different ‘flags’, focussing on subtypes of AML with the poorest prognosis.
“We know ZEB1 is also a useful tool to distinguish between relatively more and less aggressive forms of AML alike.” He said this will help “deconstruct the biological and clinical complexity observed in this disease.”
Dr Rodrigues said AML could be likened to weeds; since current treatments for AML don’t remove the ‘roots’ of the disease, the disease often returns, like weeds do when the roots have not been eradicated. Dr Rodrigues continued: “The aim of this research project is to find new therapeutics that will take aim at the ‘roots’ of AML which underpin therapy resistance and relapse.
“This is an important area of research for patients afflicted by AML where treatment strategies and prognosis have not advanced significantly for many decades. It is very difficult to speak to families who donate to our research about why AML prognosis has remained poor despite a tremendous research effort worldwide, but it is important to do so to explain the challenges in treating this disease and the hopes we have for the work we are doing.”
Dr Bubici, who received the Lister Wilder Research Grant, said she was investigating why treatments for Myeloma – which was treatable, but not curable – sometimes stopped working and why the various treatments sometimes failed to differentiate between malignant and healthy cells.
In her application for the research grant, she said: “What we know so far is that Myeloma cells are dependent on nutrients, such as sugar and fat. As a result, we propose to test whether starving Myeloma cells of nutrients could be used to treat Myeloma. This could quickly provide a new treatment option for people suffering from the disease worldwide.
“We have been studying master regulators of cell metabolism, which are present in malignant cells but not in healthy cells. We have found that blocking activities of these metabolic regulators or removing them from Myeloma cells makes them susceptible to death.
“This funding will enable us to continue conducting a series of laboratory investigations to see if depriving Myeloma cells of regulators of metabolism will restore the ability of current available drugs to treat Myeloma effectively. We will collaborate with clinicians and scientists from three haematological centres in London, Leeds, and St. Gallen in Switzerland.
“If successful, our work will lead to the testing of new drugs in combination with current anti-myeloma medications in the laboratory and, if deemed, in people. We hope that our work could rapidly lead to clinical trials of new drugs, which could give people with Myeloma a better chance of survival.”
For more information about the annual research grant, click here: https://lmruk.org/research/.